There’s not a single person in the United States who would discredit the importance of our healthcare system. Compared to the rest of the world, America is an innovation leader, whether through new technologies, new business models, and the science bringing advanced, life-enhancing treatments to society which are scaling to benefit billions where resources are available that improve access to care – and the quality of that care.
Despite this, a recent study by The Peter G. Peterson Foundation reported that the United States has one of the highest healthcare costs in the world but has a lower life expectancy rate and a higher rate of excess mortality than other comparable countries. In fact, in the US, costs have been rising more rapidly during the past decades than gross domestic products, and many experts consider this increase not to be sustainable.

Dr. Amish Purohit, Co-Founder, President & Chief Health Officer at Arkos Health, a technology-driven population health company providing patient care management, shared his thoughts on the opportunity to fundamentally improve access, especially in underserved communities while driving up quality and reducing costs in a recent interview.
“I’ll start by saying that our healthcare system is the best health care system in the world,” Dr. Purohit said. “However, when it comes to outcomes, and when we’re looking at how much we spend, looking from the outside in, you wouldn’t think we had the best healthcare system in the world. We’ve got to reduce costs in this country.”
A highly accomplished physician executive and business leader, Dr. Purohit has earned an MD, MBA MHA, FAAFP, and FACHE through a diverse educational background that includes a Bachelor of Science in Public Administration from George Mason University, a Master of Health Administration from Pennsylvania State University, and a Master of Business Administration from Kellogg School of Management at Northwestern University.
He was most recently recognized as a recipient of the Phoenix Titan 100 Award, an annual honor that recognizes executives who demonstrate exceptional leadership, vision, and passion, which Dr. Purohit has greatly displayed as he works to create a more affordable and accessible healthcare system.
“There’s no way we can sustain more than 20 or 21% of our GDP just on healthcare, or more if it continues to rise,” he continued. “If our percentage of GDP spent on healthcare goes to where it takes away money from other governmental programs that we need, like infrastructure and education, it simply makes the spending more unsustainable.”
Purohit explained that to lessen the burden of cost that healthcare imposes upon patients, there must be systemic changes to how government policies assist provider burnout, as well as the currently flawed Medicare and Medicaid reimbursement formula.
“For example, the way our government and programs around Medicaid work often amounts to a free-for-all all if you’re on Medicaid,” Dr. Purohit explained. “You’ve got free health care, you don’t have copays, and you have no other responsibility, so there’s nothing really pushing them to change their behavior patterns to use health care resources appropriately. Costs are going up, and their health outcomes are not any better.”
Instead, there are too many other determinants, such as social determinants of health (SDOH), that make it tough for Medicaid populations to prioritize healthcare. These wide-scale issues help drive the increasing cost of healthcare, making it difficult for patients to make healthcare a priority, ultimately leading to worse outcomes.
A recent Boston Globe study that found the average net worth of a black American family in the city of Boston to be just eight dollars. In reference to that finding, Dr. Purohit wonders how any family could put an emphasis on healthcare, already knowing they can’t afford it.
“These are all barriers that are created for individuals lower on the socioeconomic ladder that it becomes hard to prioritize health care,” he explained. “If they can’t prioritize health care, this correlates to poor outcomes. Just because we may have the best health care system in the world, if they’re not able to access it, they’re not able to follow through.”
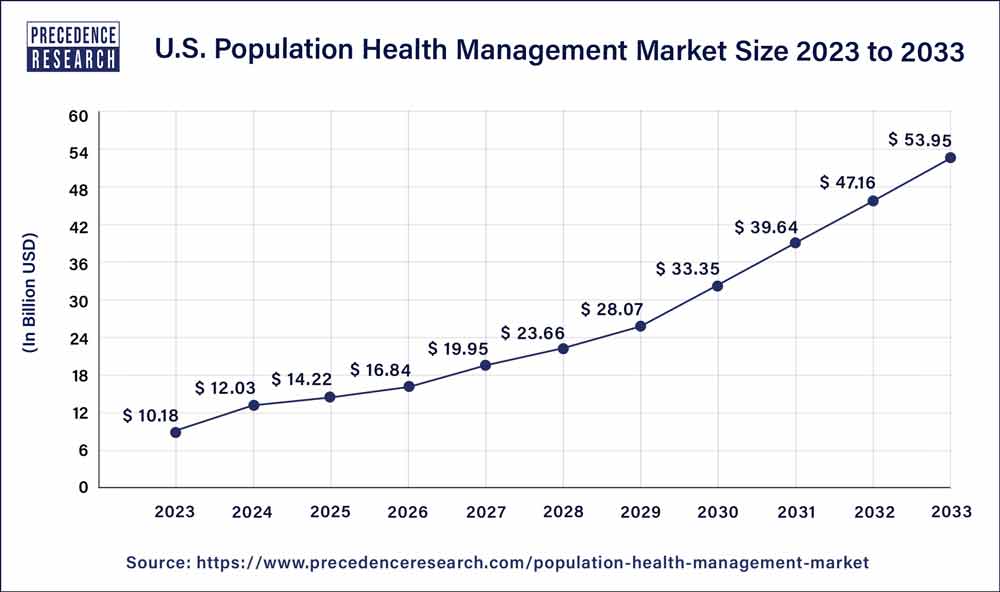
Credit: Precedence Research
Along with broad policy changes, Dr. Purohit advocates strongly for the betterment of patient education. He explains that patient education is paramount to letting people play a bigger role in their own health.
“The other piece to solving the healthcare puzzle is not only providing coverage, access, equitable, and equity in healthcare, but it is about empowering our patients and educating our patients to take ownership of their own healthcare.”
“They can’t take ownership if, on average, a person sees their doctor maybe four times a year,” Dr. Purohit said. “It’s about an hour a year if you calculate the time that they spend with their physician. If that’s the case, how can you provide better outcomes if that’s all you’re doing.”
To create greater patient empowerment, while decreasing costs at the same time, Dr. Purohit believes the answer lies with population health management and value-based care (VBC) methods and policies, like those employed by Arkos Health.
“That’s why systems like Arkos Health, where there is a higher touch point, higher access, higher availability to clinical knowledge and clinical advice for these patients, can fill those gaps in between when they see their doctors. It’s why I think there needs to be an overhaul,” he stated.
Both approaches to healthcare aim to improve the overall health outcomes of a community by the optimization of resources, including digital ones. The two approaches focus on enhancing patient outcomes by incentivizing quality over quantity and leveraging practices such as preventive care, care coordination, telehealth, patient education, and even data analytics.

The sweeping desire for change across the country, coupled with the surge in the prevalence of chronic diseases and a growing aging population, is driving the rapid growth of the population health management market, with experts predicting a promising 19.93% CAGR, bringing the 2031 estimates to a whopping USD 171.94 billion.
However, if Dr. Purohit’s beliefs prove true, population health management, as well as VBC, could very well be on the rise faster than expected as the country begins to realize that changes are necessary for the American health system to achieve world-class status.
“Our healthcare system is broken,” he said, “and the only solutions that I see right now until we fix and overhaul our entire healthcare system are solutions like Arkos Health. Population health management and value-based care companies that will help insurers to reduce costs and improve outcomes. We offer individualized care at scale. Supporting patients hand-in-hand. We coordinate care for them, wrap them with ample supporting services that impact their health, and generally drive a better experience. We’re getting paid by their insurers to put them at the center of their care because the health plans and current ecosystem of care can’t do it alone.” Learn more about Dr. Purohit on LinkedIn, and learn more about Arkos Health on their website.






